The Future of Cancer Treatment: How Immunotherapy is Achieving Remission
The future of cancer treatment is being reshaped by immunotherapy, a revolutionary approach that harnesses the body’s own immune system to target and destroy cancer cells, offering the potential for long-term remission and improved outcomes for patients.
Is the fight against cancer entering a new era? With the future of cancer treatment: exploring the potential of immunotherapy to achieve remission, this once-distant possibility is becoming a tangible reality. Let’s delve into how this innovative approach is changing the landscape of oncology.
Understanding Immunotherapy: A New Paradigm in Cancer Treatment
Immunotherapy is a type of cancer treatment that uses the body’s immune system to fight cancer. Unlike traditional therapies like chemotherapy and radiation, which directly target cancer cells, immunotherapy works by enhancing the immune system’s ability to recognize and destroy cancer cells. This approach has shown remarkable success in treating various types of cancer, offering new hope for patients.
The human immune system is a complex network of cells, tissues, and organs that work together to defend the body against foreign invaders, such as bacteria, viruses, and abnormal cells. However, cancer cells can evade detection by the immune system through various mechanisms. Immunotherapy aims to overcome these defenses and unleash the power of the immune system to eradicate cancer.
How Immunotherapy Works
Immunotherapy employs several strategies to boost the immune response against cancer. These include:
- Checkpoint Inhibitors: These drugs block “checkpoint” proteins on immune cells that prevent them from attacking cancer cells. By blocking these checkpoints, the immune system can mount a stronger response.
- T-cell Transfer Therapy: This involves extracting T cells (a type of immune cell) from a patient’s blood, modifying them in the laboratory to better recognize cancer cells, and then infusing them back into the patient.
- Monoclonal Antibodies: These are laboratory-produced antibodies designed to bind to specific proteins on cancer cells, making them more visible to the immune system or directly inhibiting their growth.
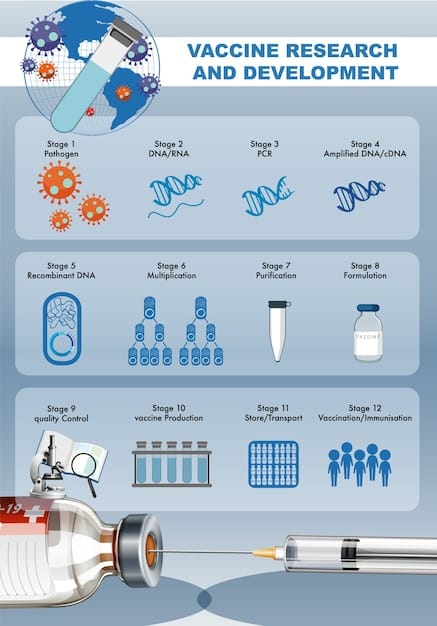
- Cancer Vaccines: These vaccines stimulate the immune system to recognize and attack cancer cells. They can be preventative (to reduce the risk of cancer development) or therapeutic (to treat existing cancer).
Immunotherapy has demonstrated significant efficacy in treating various cancers, including melanoma, lung cancer, leukemia, and lymphoma. However, it is essential to note that not all patients respond to immunotherapy, and responses can vary depending on the type and stage of cancer, as well as individual patient characteristics.
The Promise of Immunotherapy: Achieving Remission and Beyond
One of the most exciting aspects of immunotherapy is its potential to achieve long-term remission in cancer patients. Remission refers to the reduction or disappearance of signs and symptoms of cancer. While traditional treatments can often induce remission, cancer cells may eventually develop resistance, leading to relapse. Immunotherapy, on the other hand, can create a sustained immune response that continues to target and control cancer cells over the long term.
Several studies have shown that immunotherapy can lead to durable remissions in a subset of patients with advanced cancers. For instance, checkpoint inhibitors have demonstrated remarkable long-term survival rates in patients with melanoma and lung cancer, even after the treatment has been discontinued.
Long-Term Benefits of Immunotherapy
The long-term benefits of immunotherapy extend beyond just achieving remission. These include:
- Improved Quality of Life: Immunotherapy often has fewer side effects compared to traditional treatments like chemotherapy and radiation. This can translate to a better quality of life for patients during and after treatment.
- Personalized Treatment Approaches: Immunotherapy can be tailored to individual patients based on their unique characteristics and the specific type of cancer they have. This personalized approach can lead to more effective outcomes.
- Potential for Combination Therapies: Immunotherapy can be combined with other treatments, such as chemotherapy, radiation, and targeted therapies, to enhance their effectiveness and overcome resistance.
While immunotherapy offers tremendous promise, it is not without its challenges. Some patients may experience immune-related side effects, such as inflammation of the skin, lungs, or intestines. However, these side effects can often be managed with supportive care and immunosuppressive medications.
Challenges and Future Directions in Immunotherapy Research
Despite the significant advances in immunotherapy, several challenges remain that need to be addressed to further improve its effectiveness and expand its applicability. These challenges include:
Predicting which patients will respond to immunotherapy is a major hurdle. Currently, there are no reliable biomarkers or tests that can accurately predict treatment response. Researchers are actively investigating potential biomarkers, such as genetic mutations, immune cell profiles, and tumor microenvironment characteristics, to identify patients who are most likely to benefit from immunotherapy.
Overcoming Challenges in Immunotherapy
To overcome these challenges and advance the field of immunotherapy, researchers are pursuing several key directions:
- Developing New Immunotherapeutic Agents: Scientists are constantly working to discover and develop new immunotherapeutic agents that can target different pathways in the immune system and overcome resistance mechanisms.
- Identifying Novel Biomarkers: Research efforts are focused on identifying biomarkers that can predict treatment response and guide patient selection for immunotherapy.
- Improving Combination Therapies: Clinical trials are evaluating the safety and efficacy of combining immunotherapy with other treatments, such as chemotherapy, radiation, and targeted therapies, to enhance their effectiveness.
The future of immunotherapy research is bright, with ongoing efforts to address these challenges and unlock its full potential. As our understanding of the immune system and cancer biology deepens, we can expect to see further advances that will transform the way we treat cancer.

The Role of Personalized Medicine in Immunotherapy
Personalized medicine, also known as precision medicine, is revolutionizing cancer treatment by tailoring therapies to individual patients based on their unique genetic and molecular characteristics. This approach is particularly relevant to immunotherapy, as it can help identify patients who are most likely to respond to specific immunotherapeutic agents and guide treatment decisions.
Genetic testing and molecular profiling can reveal mutations and alterations in cancer cells that may make them more susceptible to immunotherapy. For example, certain mutations in genes involved in DNA repair or immune evasion can predict a better response to checkpoint inhibitors.
Benefits of Personalized Immunotherapy
The benefits of personalized immunotherapy include:
- Improved Treatment Outcomes: By selecting the right immunotherapeutic agent for the right patient, personalized medicine can improve treatment outcomes and increase the chances of achieving remission.
- Reduced Side Effects: Personalized medicine can help avoid unnecessary exposure to immunotherapeutic agents that are unlikely to be effective, reducing the risk of side effects.
- Cost-Effectiveness: By targeting treatment to patients who are most likely to benefit, personalized medicine can improve the cost-effectiveness of immunotherapy.
Personalized medicine is transforming the field of immunotherapy, paving the way for more effective and tailored cancer treatments. As our understanding of cancer biology and the immune system continues to advance, we can expect to see even more sophisticated approaches to personalized immunotherapy in the future.
Clinical Trials: Advancing the Future of Immunotherapy
Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, including immunotherapy. These trials involve testing new therapies on patients with cancer under carefully controlled conditions. Clinical trials provide valuable data that can help determine whether a new treatment is safe and effective, and whether it should be approved for use in clinical practice.
For immunotherapy, clinical trials are crucial for identifying the best ways to use these treatments, determining the optimal doses, and understanding which patients are most likely to benefit. Clinical trials also help researchers to identify and manage potential side effects of immunotherapy.
Participating in Clinical Trials
Participating in a clinical trial can offer several benefits to patients with cancer, including:
- Access to Cutting-Edge Treatments: Clinical trials often provide access to new immunotherapeutic agents that are not yet available to the general public.
- Close Monitoring and Care: Patients participating in clinical trials receive close monitoring and care from a team of healthcare professionals.
- Contribution to Medical Advancement: By participating in a clinical trial, patients can contribute to the advancement of medical knowledge and help improve cancer treatment for future generations.
Clinical trials are crucial for advancing the future of immunotherapy. By participating in these trials, patients can access cutting-edge treatments, receive close monitoring and care, and contribute to the advancement of medical knowledge.
The Economic and Societal Impact of Immunotherapy
The advent of immunotherapy has not only transformed the landscape of cancer treatment but has also had a significant economic and societal impact. While the initial costs of immunotherapy can be high, the long-term benefits, such as improved survival rates and reduced need for other treatments, can outweigh these costs.
From a societal perspective, immunotherapy can lead to increased productivity and reduced healthcare costs associated with long-term cancer care. Immunotherapy can also empower patients with cancer to live longer, healthier lives, contributing to their families and communities.
Future Impact of Immunotherapy
The future economic and societal impact of immunotherapy is expected to be substantial. As more immunotherapeutic agents become available and the cost of treatment decreases, more patients will have access to these life-saving therapies. This will lead to:
- Reduced Cancer Mortality Rates: Immunotherapy has the potential to significantly reduce cancer mortality rates, leading to a healthier and more productive population.
- Increased Economic Productivity: By enabling patients with cancer to live longer, healthier lives, immunotherapy can increase economic productivity and reduce the burden of cancer on society.
- Innovation in Healthcare: The success of immunotherapy is driving innovation in healthcare, leading to the development of new and more effective cancer treatments.
Immunotherapy is not just a medical breakthrough—it’s an economic and societal game-changer. As we continue to unlock its potential, we can expect to see profound and positive changes in the lives of patients with cancer and society as a whole.
| Key Point | Brief Description |
|---|---|
| 🔬 Immunotherapy | Uses the body’s immune system to fight cancer. |
| ✅ Remission | Offers potential for long-term reduction or disappearance of cancer signs. |
| 🧬 Personalized Medicine | Tailors treatments based on individual genetic and molecular traits. |
| 🧪 Clinical Trials | Essential for evaluating the safety and efficacy of new immunotherapies. |
FAQ on Immunotherapy
▼
Immunotherapy enhances the patient’s immune system to fight cancer. It differs from chemotherapy by targeting the immune system, not the cancer cells directly, thus enabling the body to recognize and destroy cancer.
▼
Immunotherapy shows promise in treating various cancers, including melanoma, lung cancer, leukemia, and lymphoma. Its effectiveness varies based on the type and stage of the cancer, as well as individual patient factors.
▼
Common side effects include inflammation of the skin, lungs, or intestines. These are generally manageable with supportive care and immunosuppressive medications, but it’s crucial to monitor and report any changes to healthcare providers.
▼
Personalized medicine customizes treatments based on an individual’s genetic and molecular profile. This approach maximizes the likelihood of a positive response and reduces exposure to ineffective treatments, optimizing the immunotherapy process.
▼
Clinical trials are essential to assess the safety and efficacy of new immunotherapies. They offer patients access to cutting-edge treatments and contribute valuable data that guide future advancements in cancer treatment protocols.
Conclusion
The future of cancer treatment: exploring the potential of immunotherapy to achieve remission represents a paradigm shift in oncology, offering hope for long-term remission and improved quality of life for patients. While challenges remain, ongoing research and clinical trials are paving the way for more effective and personalized immunotherapeutic approaches that will continue to transform the fight against cancer.





