Antibiotic Resistance: A National Health Crisis in the US?

The rise in antibiotic-resistant infections is increasingly recognized as a significant national health crisis in the US, threatening to reverse decades of progress in treating common infections. This issue demands immediate attention and comprehensive strategies to mitigate its impact and prevent future outbreaks.
Is the rise in antibiotic-resistant infections a national health crisis? Expert Analysis and Prevention Strategies are critical to understanding and combating this growing threat which impacts communities across the United States.
Antibiotic Resistance: Understanding the Threat
Antibiotic resistance is a naturally occurring phenomenon where bacteria evolve to withstand the effects of antibiotics. However, its acceleration due to overuse and misuse of antibiotics has turned it into a pressing public health concern, especially in the US.
What is Antibiotic Resistance?
Antibiotic resistance happens when bacteria change in a way that reduces or eliminates the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The resistant bacteria survive and continue to multiply, causing more harm.
Why is it a Growing Problem?
The overuse and misuse of antibiotics in human medicine and animal agriculture are major drivers of antibiotic resistance. When antibiotics are used unnecessarily, bacteria are exposed to these drugs, increasing the likelihood of resistance developing.
- Overuse in Humans: Prescribing antibiotics for viral infections like colds and flu.
- Agricultural Use: Using antibiotics in livestock for growth promotion and disease prevention.
- Lack of Infection Control: Inadequate hygiene and sanitation practices in healthcare facilities and communities.
Understanding the mechanisms and causes of antibiotic resistance is the first step toward addressing this complex problem. Further research, stricter regulations, and responsible antibiotic use are crucial to slowing down the emergence and spread of resistant bacteria.
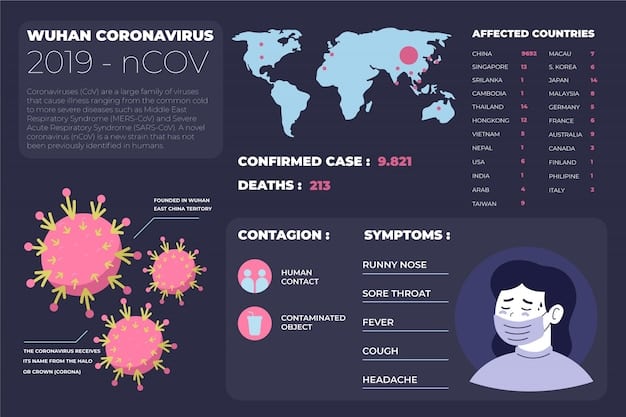
The Scope of Antibiotic-Resistant Infections in the US
The impact of antibiotic-resistant infections in the United States is substantial, affecting millions of people annually and resulting in significant healthcare costs and mortality. Understanding the scope of the problem is crucial for prioritizing interventions and resource allocation.
Incidence and Prevalence
According to the Centers for Disease Control and Prevention (CDC), antibiotic-resistant infections cause millions of illnesses and tens of thousands of deaths in the US each year. The prevalence of specific resistant bacteria varies by region and healthcare setting.
Affected Populations
Certain populations are more vulnerable to antibiotic-resistant infections, including:
- Hospitalized Patients: Individuals in hospitals are at higher risk due to frequent antibiotic use and invasive procedures.
- Elderly: Older adults often have weakened immune systems and chronic conditions, making them more susceptible.
- Individuals with Compromised Immunity: People with HIV/AIDS, cancer patients, and transplant recipients face an elevated risk.
Economic Burden
The economic burden of antibiotic-resistant infections is substantial, with estimated costs running into billions of dollars annually. These costs include:
The increase in healthcare expenditures because of antibiotic-resistant infections extends to the development and research of new antibiotics, as well as the implementation of comprehensive infection control practices aiming to prevent the spread of these resistant pathogens across healthcare environments.
- Prolonged Hospital Stays: Infections with resistant bacteria often require longer hospital stays, increasing healthcare costs.
- Expensive Treatments: Newer, more expensive antibiotics may be necessary to treat resistant infections.
- Increased Mortality: Higher mortality rates associated with resistant infections lead to loss of productivity and reduced quality of life.
Addressing antibiotic resistance requires a multi-faceted approach involving healthcare providers, policymakers, researchers, and the public. Enhanced surveillance, antibiotic stewardship programs, and investment in research and development are essential for mitigating the impact of these infections.
Public Health and Safety
The rise in antibiotic-resistant infections introduces significant challenges to public health, demanding robust surveillance systems, effective infection control practices, and stringent regulatory oversight to mitigate the spread and impact of these infections on communities across the United States.
Surveillance Systems
Effective surveillance systems are crucial for monitoring the prevalence and spread of antibiotic-resistant bacteria. These systems allow public health officials to identify outbreaks, track trends, and implement targeted interventions.
Infection Control Practices
Infection control practices are vital for preventing the transmission of antibiotic-resistant bacteria in healthcare settings and communities. Key strategies include:
- Hand Hygiene: Frequent and thorough hand washing with soap and water or using alcohol-based hand sanitizers.
- Isolation Precautions: Isolating patients with resistant infections to prevent transmission to others.
- Environmental Cleaning: Regularly cleaning and disinfecting surfaces and equipment in healthcare facilities.
Regulatory Oversight
Stringent regulations are necessary to ensure the appropriate use of antibiotics in human medicine and animal agriculture. This includes:
The Role of Vaccination
Vaccination plays an important role in safeguarding public health by reducing the demand for antibiotics. Vaccines prevent bacterial infections and protect populations against diseases that could lead to overuse and resistance.
- Antibiotic Stewardship Programs: Programs that promote the appropriate use of antibiotics in healthcare settings.
- Restrictions on Agricultural Use: Limiting the use of antibiotics in livestock for growth promotion.
- Monitoring and Enforcement: Regularly monitoring antibiotic use and enforcing regulations to prevent misuse.
Vaccination presents a strategic approach to lessening the burden on antibiotics, thereby helping to slow down resistance and preserve efficacy for severe bacterial infections.
Expert Analysis: Causes and Contributing Factors
Understanding the causes and contributing factors behind the rise in antibiotic-resistant infections is essential for developing effective prevention and control strategies. Experts emphasize the complex interplay of factors driving this growing threat.
Overuse of Antibiotics
The overuse of antibiotics in human medicine is a primary driver of antibiotic resistance. Prescribing antibiotics for viral infections, such as colds and flu, is a common example of inappropriate use.
Misuse in Agriculture
The agricultural sector significantly contributes to the development of antibiotic resistance due to the widespread use of these drugs in livestock. This misuse accelerates the emergence and spread of resistant bacteria.
The overuse and misuse of antibiotics in animal agriculture also plays a significant role. Antibiotics are often used in livestock for growth promotion and disease prevention, leading to the development of resistance.
The misuse of antibiotics in agriculture includes:
- Growth Promotion: Using antibiotics as growth promoters in livestock feed.
- Preventive Use: Administering antibiotics to animals to prevent disease, even in the absence of infection.
- Subtherapeutic Doses: Exposing bacteria to low doses of antibiotics, increasing the likelihood of resistance development.
Cross-Resistance and Co-Resistance
Cross-resistance and co-resistance are mechanisms by which bacteria develop resistance to multiple antibiotics simultaneously. This can occur when resistance genes are located close together on mobile genetic elements.
In summary, addressing the causes and contributing factors of antibiotic resistance requires a comprehensive approach involving education, regulation, and research. Collaboration between healthcare professionals, policymakers, and the public is essential for preserving the effectiveness of antibiotics.
Prevention Strategies and Best Practices
Effective prevention strategies and best practices are crucial for combating the rise in antibiotic-resistant infections. Emphasizing responsible antibiotic use, enhancing infection control, and promoting vaccination are key components of a comprehensive approach.
Responsible Antibiotic Use
Promoting responsible antibiotic use is essential for preserving the effectiveness of these drugs. Key strategies include:
Initiatives like public awareness campaigns and enhanced professional training offer vital support. These methods empower individuals to make well-informed choices about antibiotic usage and enhance the general knowledge surrounding appropriate prescriptions.
- Avoiding Unnecessary Prescriptions: Prescribing antibiotics only when they are truly necessary, based on clinical guidelines.
- Using Narrow-Spectrum Antibiotics: Selecting antibiotics that target specific bacteria, rather than broad-spectrum drugs.
- Completing the Full Course: Ensuring that patients complete the full course of antibiotics, even if they start feeling better.
Enhanced Infection Control
In order to promote enhanced sanitation procedures, it is essential to adopt extensive hygiene promotion programs, especially in settings such as healthcare institutions and educational facilities. These programs play a crucial role in reducing the transmission of resistant microorganisms.
### Vaccination for Prevention
Vaccination is a powerful tool for preventing bacterial infections and reducing the need for antibiotics. Vaccines can protect against diseases such as pneumonia, influenza, and meningitis, which can often lead to antibiotic use.
Effective infection control practices are necessary to prevent the transmission of antibiotic-resistant bacteria in healthcare settings and communities. This includes:
- Hand Hygiene: Regular hand washing with soap and water or using alcohol-based hand sanitizers.
- Isolation Precautions: Isolating patients with resistant infections to prevent transmission to others.
- Environmental Cleaning: Regularly cleaning and disinfecting surfaces and equipment.
Implementing comprehensive vaccination agendas protects against bacterial illnesses, diminishing the necessity for antibiotics and contributing to minimize resistance.
Future Directions and Research Innovations
The future of combating antibiotic resistance relies on continued research, innovation, and global collaboration. Exploring new therapies, improving diagnostics, and enhancing surveillance are essential for staying ahead of this evolving threat.
Novel Therapies
Research into novel therapies is crucial for developing new treatments for antibiotic-resistant infections. Various approaches are being explored, including:
- Bacteriophage Therapy: Using viruses that infect and kill bacteria to treat infections.
- Antimicrobial Peptides: Developing small peptides that disrupt bacterial cell membranes.
- Immunotherapies: Harnessing the immune system to fight bacterial infections.
The advent of innovative therapeutic approaches presents promising pathways for coping with antibiotic resistance, paving the way for targeted treatments that diminish dependence on traditional antibiotics and mitigate the development of further resistance.
Improved Diagnostics
Rapid and accurate diagnostics are essential for guiding antibiotic therapy and preventing the unnecessary use of antibiotics. Advances in diagnostic technologies include:
International Cooperation
Combating antibiotic resistance requires international cooperation and collaboration. Sharing data, coordinating research efforts, and harmonizing regulatory standards are essential for addressing this global threat.
The improvement of diagnostic technologies allows healthcare providers to pinpoint infections rapidly and administer ideal antibiotics, reducing overuse and optimizing treatments for enhanced patient results.
Key Point
Brief Description
🔑 Antibiotic Resistance
Bacteria evolve, becoming resistant to antibiotics, threatening treatment efficacy.
🛡️ Prevention Strategies
Includes responsible antibiotic use, enhanced infection control, and vaccination.
🔬 Research Innovations
Exploring novel therapies like bacteriophages and improving diagnostics.
🌍 Global Cooperation
Essential for data sharing, research coordination, and harmonizing regulations.
Frequently Asked Questions
Antibiotic resistance happens when bacteria evolve to survive exposure to antibiotics, reducing or eliminating the drug’s effectiveness in treating infections.
It makes infections harder to treat, increasing the risk of severe illness and mortality. It also leads to higher healthcare costs and prolonged hospital stays.
Use antibiotics only when prescribed, complete the full course of medication, practice good hygiene, and get vaccinated to prevent bacterial infections.
The use of antibiotics in livestock for growth promotion and disease prevention contributes to the development and spread of antibiotic-resistant bacteria.
These are programs that promote the appropriate use of antibiotics in healthcare settings, ensuring they are prescribed only when needed and for the correct duration.
Conclusion
In conclusion, the rise in antibiotic-resistant infections constitutes a significant national health crisis in the US, demanding urgent attention and comprehensive strategies to mitigate its impact. By understanding the causes, implementing effective prevention measures, and investing in research and innovation, we can work towards preserving the effectiveness of antibiotics and safeguarding public health for future generations.
Read more content





